6.1 Introduction
Through this unit you will learn basics about trauma and how it affects a person’s functional ability, health and quality of life. We will review the symptoms of traumatization and, in particular, how it affects arousal regulation[1]. The unit also provides ways to optimize your own and your customer’s alertness regulation. At the end of the unit, it is explained how homelessness and trauma intertwine and why violence in particular is related to trauma among homeless people.
6.2 Learning objectives
In this unit the learners will
- Understand what is trauma
- Learn about different types of trauma
- Become acquainted with the concept of the Window of Tolerance
- Learn about symptoms of trauma
- Acquire tools for working with traumatized people
- Understand why homelessness is a traumatic incident
- Understand how experiences of violence cause trauma
6.3 What is trauma?
Trauma is a damage caused by force majeure. A traumatic crisis is a sudden, surprising, and unusually powerful event that would cause suffering to anyone. Traumatization occurs when an individual simply does not find ways to protect themselves from the pain caused by a traumatic event. Mental pain is too intense, and events lock into the persons mind and body. In addition to the traumatic event happening to oneself, witnessing another person’s traumatic experience can also be traumatic. Sometimes it is not about what has happened but what has been left out. An example of this is the lack of care in childhood.
Trauma is an escape and concealment in nature: the traumatized persons typically seek to avoid and deny what has happened and experience shame and guilt. Severity or level of trauma is affected by the intensity and duration of the event, frequency, unpredictability, uncontrollability. The accumulation of stressors, lack of care and social support, and emotional abuse also predispose to trauma. It is also known that women are more affected by trauma than men.
Usually, the trauma is activated regardless of the will and causes the person who experiences it a deep anxiety and a feeling of not being able to control their own body or mind. Triggers are closely related to the cause of trauma. There are stimuli that trigger a traumatic experience or memory. These stimuli can be anything: a smell, a sound, a look from another person, the way someone touches you, or a particular event.
If the brain is exposed to intense stress during childhood permanent nervous changes can occur. This means that a traumatized person is more prone to experience stress than a person who hasn’t been exposed to traumatizing events. Stress also activates a more physically emergency state. Therefore, a traumatized person may have difficulty regulating their own feelings and even small things may derail normal life.

Trauma can be divided into two groups:
Type 1 refers to single-incident traumas which are unexpected and come out of the blue.
Type 2 refers to complex trauma which may have been experienced during childhood or early stages of development. Type 2 trauma also develops from repetitive and long-lasting traumatic experiences.
| EXAMPLES OF TRAUMA | EXAMPLES OF TRAUMA |
|---|---|
| TYPE 1 | TYPE 2 |
| · Severe illness or injury · Violento or sexual assault · Mugging or robbery · Being a victim or witness to violence · Witnessing a terrorist attack, a natural disaster, etc. · Road accident · Military combat incident · Hospitalisation and psychiatric hospitalisation · Childbirth · Medical trauma · Post suicide attempt trauma · Life threatening illness or diagnosis | · Childhood emotional abuse · Domestic violence · Emotional neglect and attachment trauma · Abandonment · Verbal abuse · Coercion · Domestic physical abuse · Long term misdiagnosis or a health problem · Bullying at home or school or in a work environment · Emotional and sexual abuse · Physical neglect · Overly strict upbringing sometimes religious |
What does trauma do to a person?
In general, a healthy person believes that the world is good, life is purposeful, and people are valuable. A traumatic event threatens a person’s belief system. A shocking event can even crush the belief system because it happens unpredictably and haphazardly. The illusion of invulnerability disappears and the person loses the sense of control.
Traumatic experiences are specific to the human psyche because they are stored in memory unlike everyday events. When an individual finds himself in a highly stressful situation, his body secretes endogenous hormones called stress hormones that reinforce the memory of a traumatic situation. Traumatic memories are recorded, at least in part, in a non-linguistic form as images, smells, emotions, and sounds. In a traumatic crisis, it is a matter of loss: the loss of one’s health, one’s loved one, one’s lifestyle, or the meaning of life. It is therefore natural that a crisis can cause feelings of sadness, guilt, hopelessness and shame. Facing a traumatic crisis requires a lot of mental resources and physical endurance.
Trauma symptoms may include physical, mental or social symptoms of almost any kind, as well as symptoms related to affect regulation. Symptoms can be for example attention deficits, absent-mindedness, blackouts, addictions, panic attacks, eating disorders, physical pain and numbness, tendency to mistrust, hallucinations, depression and fatigue. Considering this diversity, it is unsurprising that trauma patients get multiple varying psychiatric diagnoses on the way. Trauma and its symptoms affect human functioning extensively. Of the many different symptoms, we have chosen the following to focus on: 1. arousal regulation problems, 2. difficulties in interpersonal relationships, 3. emotions and detachment, 4. addictions and self-destructive behavior.
- Arousal regulation problems
Arousal regulation problems are very typical symptoms of trauma. Understanding them is very important when meeting a person with traumatic experiences. It is good to remember that the professional’s arousal regulation also varies and it is important that the professional is in optimistic arousal during meetings with the clients.
WINDOW OF TOLERANCE
Window of tolerance is a term used to describe the zone of arousal in which a person is able to function most effectively. When people are within this zone they are typically able to readily receive, process and integrate information and otherwise respond to the demands of everyday life without much difficulty. This optimal window was first named as such by Dan Siegel.
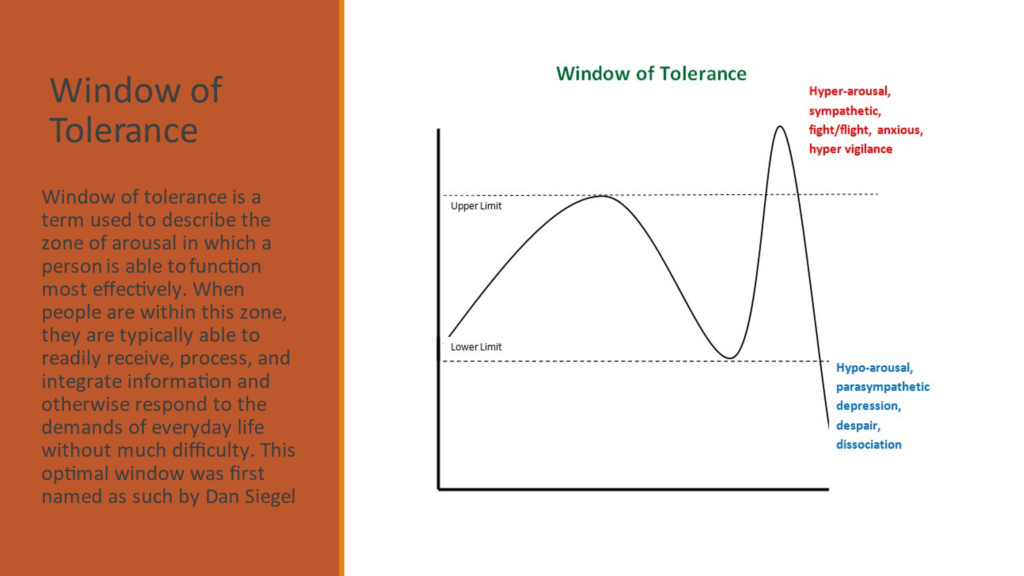
In the hypoaroused state the parasympathetic nervous system is preparing for a potential death, and the body prepares to play dead. A constant state of hypoarousal can easily lead to isolation and prolongation of paralysis. A functional means of controlling hypoarousal in a triggering situation would be activating the body and anchoring in the present moment. Feelings of emptiness, exhaustion, lack of thoughts, sluggishness and decreased functional capacity may make life isolated. Life goes on in “slow motion”. Hypoarousal as a trauma mechanism is related to the narrowing of consciousness, in response to situations that have been overpowering for the person, sometimes already in their childhood. For someone unfamiliar with trauma, hypoarousal behavior may appear to be a lack of motivation, which in turn may affect the cooperation between the homeless person and the service provider.
For example, in childhood, paralysis may develop as a coping strategy in overwhelming situations, where submission is the only chance of minimizing harm. Paralysis as a trauma symptom is usually a childhood survival strategy, turning into a counterproductive symptom in adulthood, while the conditions and environment have changed. As a reaction to trauma, hiding under a blanket may look like inappropriate in adulthood but is regarded as the only “sensible” strategy or in fact an automatized pattern of the nervous system by the parts that remain in the trauma reality.
The opposite of hypoarousal is hyperarousal, where the state of fight or flight is activated by sympathetic nervous system. In the state of hyperarousal, breathing and heart rate are increased, senses are sharpened, and the body is prepared to run. Many traumatized individuals live in a state of constant tension. A reminder of trauma may lead to a difficult and anxious state of mind, which can be hard to get out of, understand or describe. Symptoms may include: chronic anxiety, difficulty falling or staying asleep, difficulty concentrating, irritability, anger and angry outbursts, panic attacks and being constantly on guard for threats.
Many who have worked with people who have experienced homelessness will certainly recognize a client who suddenly becomes nervous and agitated, and may want to leave the place. This does not mean that the professional necessarily did anything wrong. Something in a meeting, such as the professional’s voice or an uncomfortable meeting place for a client, can trigger a trauma memory. A sudden reaction may surprise both the professional and the client and the client may be misinterpreted as prickly and violent.
2. Difficulties in interpersonal relationships
In their relationships, traumatized individuals often face many challenges and complexities. These complexities are related to the lack of experience of reliable and secure relationships. They simply haven’t had a chance in life to learn how normal relationships work, how to stand for themselves and disagree with others sometimes, how to listen and be heard, how to apologize and to forgive, and go on after together.
Fundamentally, what relationship complexities are all about, is trust that has been broken or almost destroyed. The childhood environment of a traumatized individual has required constant vigilance, threat detection and fear of the worst. The traumatized person seeks to anticipate threat and danger and, as a result, easily finds those things in the gestures, expressions and words of others all the time. Because of traumatization, normal abilities in detecting threat and danger may have become so distorted that we are not able to discern people that are safe for us from those who are not. This course of interpretation easily leads to isolation and withdrawal from relationships, which eventually pushes other people even farther away.
Acquiring new interpersonal skills demand great activeness and introspection concerning one’s own contributions, so that one can begin to improve the quality of their relationships and get a chance for compensatory experiences. The patterns of thought and action can be explored together with safe people. In general, it is possible to think that, usually, people have good intentions. Because the nervous system works faster than the brain, the skill of apologizing is an adept one.
3. Emotions and detachment
Many traumatized people describe losing touch with their own feelings. Frequently, emotional detachment may be linked to describing traumatic events, or some other consciously or unconsciously stressful situation. For others, detachment is something normal in their everyday lives. They have isolated emotions somewhere outside their awareness, so that feelings can’t activate properly in everyday life, no matter how natural that would be.
Some people feel like their life is nothing but strong emotions and find themselves swinging from one extreme to another. For some, emotions are completely lacking. Alternatively, some may fall into a state of no emotion, and in the next instant, become extremely emotional. More slight or intermediate emotions may be difficult to recognize.
The threat-detecting autonomic nervous system of a traumatized individual is operating faster than the conscious mind, so that responses to various situations— e.g. regarding other people— are not always appropriate.
“Often, when things go over my head, I turn perfectly calm. I analyze and talk about what happened, smiling, and I talk about myself and my experiences in a detached way, like there was a wall between, no emotional contact. It doesn’t affect me, there is no me, although I know it’s my life.”
4. Addictive and self-destructive behavior
Emotional trauma can lead to various addictions. In other words, addictions may be rooted in experiences of outsiderness, detachment, and disconnectedness, for which one is striving to find a solution. Looking for solution, the addict is getting caught in activities or substances that produce pleasure, excitement, relief, fulfilment. Addiction may show as dependence on alcohol or drugs, pornography, food, or gambling, or as well to some kind of activity or work. Addiction may be seen as an attempt to fix or alleviate an early trauma, whether unconscious or identified.
Self-destructiveness comes in many forms, including repeating traumatic events, numbing one’s emotions or escaping from self. Often, the idea in experiencing pain is to avoid some emotion or traumatic memory that would be even more painful. However irrational it seems, for the system, these malicious and angry thoughts are well-meaning. During some overpowering conditions in one’s life, the self-destructive part has served in protecting the other parts by hurting oneself. However, in adult life, there is a much larger range of coping mechanisms available. In recovery, it is important for the individual to practice protecting himself and all his parts by using alternative non-destructive strategies.
In many cases, substance use is associated with homelessness, but of course not always. Even if a person did not have a substance abuse problem before homelessness, experiencing homelessness can be such a hard experience that a person tries to combat bad feelings by using intoxicants. For a person that has learned to escape her own trauma memories with intoxicants, recovery can be difficult. After sobriety, trauma experiences come back to mind and they can be difficult to face. In a situation like this, a person needs specialized help.
Tools that can be used in work with people who have experienced trauma:
- Psychoeducation (Providing information and understanding concerning a mental disorder. Information about trauma helps to manage the symptoms, and with knowledge, a person can understand their inner world better.)
- Creative methods (music, arts, etc.)
- Breathing and relaxation exercises
- Make sure that basic human needs (food, sleep, economic income, etc.) are fulfilled as well as possible
Helpful aspects when organizing and running an appointment with a client who have experienced trauma:
- Let the client choose the time and the place for appointment
- Explain how much time has been set aside for the meeting and what will be discussed. In the end, make a summary of the important things discussed/agreed upon.
- Keep a clock and a calendar in a visible place during appointments so that the client can be more time-oriented
- Make sure that the client can leave if necessary and inform him about it
- Offer the client to hold something in their hands, e.g. coffee cup, stress ball
- Memory support (sticky notes, dictating important things to your phone, support person)
- Carefully prepare for meetings with the client so that he does not have to tell many times about difficult things and situations
- Take a break between client appointments so that your own arousal is optimal

Trauma and homelessness are interlinked
Traumatizing experiences can be an important factor in many people’s pathway to homelessness. People who become homeless are likely to have experienced some form of trauma, often in childhood. Approximately an 85% of those in touch with criminal justice, substance misuse and homelessness services have experienced trauma as children.
Trauma often happens when the person is already homeless, for example by being a victim of an attack, sexual assault or any other violent event. People can also be re-traumatised by services that leave them feeling powerless and controlled; for example, if they lack privacy and are not sufficiently involved in decision making related to aspects that affect them as a service user.
Homelessness itself can be considered a traumatic experience in multiple ways. Often the loss of a home together with the loss of family connections and social roles can be traumatic. This is because “like other traumas, becoming homeless frequently renders people unable to control their daily lives”.
Homeless people experience violence. The violence faced by homeless women is particularly diverse. In the UK, as many as 95 per cent of homeless women have experienced physical violence and 80 per cent have experienced sexual violence. The figures can be expected to be similar in other countries. The experiences of violence and exploitation of many women have begun in their childhood. A domestic violence experience is common among youth, single adults, and families who become homeless. For many, it is the immediate cause of their homelessness.
“Domestic Violence can be defined as physical, sexual or psychological harm by a current/former partner or spouse as well as by other family members, or by a partner’s family members. DV can take many forms, including physical injuries, abuse and rape or mental cruelty in the form of bullying, insults or harassment. Very often, domestic violence is a combination of physical, sexual and/or emotional abuse. This type of violence can occur among heterosexual or LGBTQ2S couples and does not require sexual intimacy.”
There are various forms of violence:
- Physical violence: shoving, punching, kicking, pulling the hair, hitting the head, scratching, tearing, shaking, using a firearm or edged weapon, threatening with physical violence.
“I often sleep, with someone else, because sleeping alone is dangerous. I have been beaten many times while all my stuff has been robbed. But I have sometimes been violent myself. There are jungle laws on the street. – Man 49 years old”
- Psychological violence: subjugation, criticism, name-calling, disdain, control, restriction of social interaction, morbid jealousy, isolation, breaking things, harming pets, or threatening with any of the above or suicide.
“Now, afterwards, I have only realized what violence is all about. Throughout homelessness, I was called names by both, other homeless and passers-by. Then, I was in the clutches of one gang for a moment. If I didn’t steal for them, they threatened to kill my dog”. Woman after 8 years of homelessness
- Sexual violence: rape, attempted rape, coercion into various forms of sexual activity or sexual intercourse, threatening with sexual violence, sexual debasement, forcing into pornography, prohibiting use of contraception, forcing an abortion, restricting sexual self-determination.
“Being a homeless woman is not safe. I’m used to being touched even if I don’t want to. Sometimes I’ve got a place to sleep from some men. They often demand sex for it. A few times I have agreed because I was afraid I would be raped. Now I understand it was rape”. Woman 26 years old
- Financial violence: preventing independent use of money, preventing participation in financial decision-making or forcing the handing over of own money to another person, threatening with financial violence or blackmail.
“I never had money. I had to give the social benefits to my spouse and he gave me a little money if I needed anything. He also had my ID, which he often lost. My social worker didn’t understand why I often needed a new ID. He thought I was careless and lost it myself”. Young woman
- Stalking: repeated unwanted contacts, spreading false information, destroying property, intimidation, following, spying, theft and misuse of personal data.
“I am now in a shelter with my children. We are homeless because we cannot go back to our own home. My husband is violent and is stalking me. We have been waiting for a new home for a long time, but it is difficult to find. We need to move to another city and we cannot live in an apartment that is on the first floor because I don´t feel safe there. My social worker does not understand this”. Mother of two kids
- Abuse or negligence: leaving a child, elderly person or disabled person without care, help or treatment in situations when the victim depended on them, harming another person with drugs, intoxicants, chemicals or solvents.
“When I was a child my parents left me home alone for days. They had a substance abuse problem. I had to go to a foster home and started using drugs myself. I have not been able to take care of my own children. I gave them away because I don’t want them to experience same things I did”. Woman 44 years old, 5 years of being homelessness”
- Cultural or religious violence: forcing compliance with a religious conviction, threat of violence or use of violence with references to religion or to culture as justification, e.g. honor violence, threats rooted in religion.
“My family was very religious and we lived in a small locality. I have known since I was very young that I am gay. When I told my parents about it, they considered me sick. I was not accepted into my own religious community and had to move away from home, to a bigger city. I was alone and I didn’t know anyone. I started drinking alcohol, my studies were interrupted and I ended up homeless”. Man 39 years old
6.4 Further Reading and resources
- Gonzalez A. [IHDCYH Talks] Adverse Childhood Experiences (ACEs): Impact on brain, body and behaviour.
- McCrory E. [Anna Freud NCCF] Childhood Trauma and the Brain | UK Trauma Council.
- NHS Education for Scotland. [Positive Steps] Opening Doors Trauma Informed Practice for the Workforce.
- The Finnish Association for Trauma and Dissociation. (2018). Trauma symptoms – Causes, effects and management. Accesible en: https://www.disso.fi/wp-content/uploads/2019/11/Symptoms-of-Trauma-Dissociation.pdf
[1] the controlling of cognitive and physiological activation using cognitive behavioral methods (APA Dictionary of Psychology)






